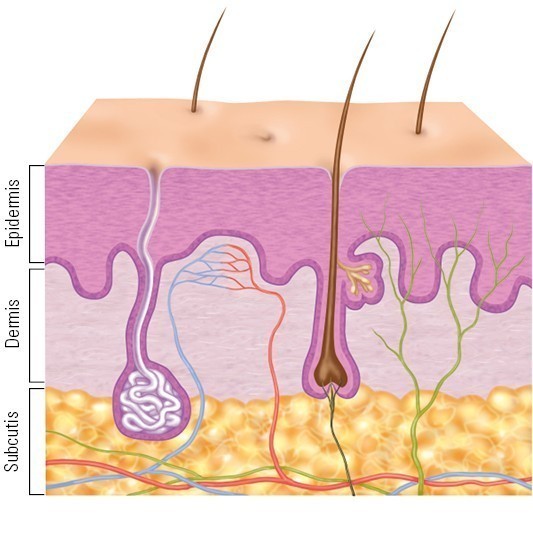
Mechanical injuries
This type of injury occurs as a result of force exerted by objects and pressure, as well as shear forces and tractive force. Mechanical injuries can result in both open mechanical wounds such as stab wounds and closed mechanical wounds such as bruises or contusions.
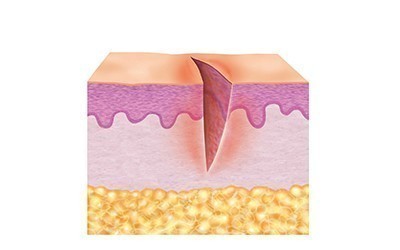
- Cuts
- Wounds from punches or blows
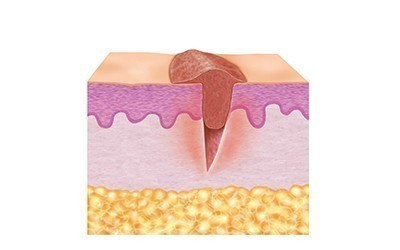
- Stab or puncture wounds
- Gunshot wounds
- Wounds from bites
- Scratches
- Lacerations
- Wounds from tears
- Wounds from abrasions
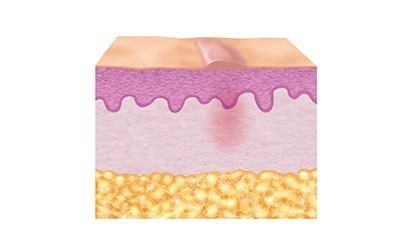
- Contusions
- Bruises
- Blisters
- Insect bites