

Venous leg ulcers (ulcus cruris venosum)
Information relating to leg ulcers
Venous leg ulcers, also known as “leg ulcers”, is a term used to refer to a serious, painful wound which generally does not heal well. You can read about key risk factors, treatment options and much more here.
Venous leg ulcers – definition
Venous insufficiency which lasts a number of years may lead to a chronic wound on the lower leg or foot. Due to the permanent backlog in the veins, oedemas develop. If oedemas are present for a longer period of time, the tissue is no longer supplied with sufficient oxygen. As a consequence, the skin becomes thinner and thinner until an open wound ultimately develops, which may become chronic without treatment. This chronic condition is often referred to as a leg ulcer by the general population or a venous leg ulcer by experts. The term ulcus cruris venosum comes from Latin. “Ulcus” means “ulcer”, “crus” means “leg” or “lower leg” and “vena” means “vein”. The plural of ulcus is “ulcera”. We tend to use the term “ulcer” in English.
Why do people get venous leg ulcers?
A venous leg ulcer generally develops slowly over a period of months or even years. It presents as damage to the skin, which manifests itself as dry, itchy or cracked skin. Over the course of time, the skin may get thinner and more susceptible to injury. If wounds which occur due to this condition do not heal properly or are not treated properly, they often get larger and deeper. The wounds may be moist or swollen and emit an unpleasant odour.

Leg ulcers: Causes
The main cause of venous leg ulcers is a chronic venous condition. This occurs when the venous valves no longer work properly. This leads to a build-up of blood in the veins and increases the pressure there. This increased pressure damages the skin and the tissue beneath it, which can lead to venous leg ulcers.
Further risk factors include the following:

Blood clot

Being overweight

Pregnancy

Insufficient physical activity

Smoking
A venous leg ulcer is often connected to a circulatory issue in the legs and pre-existing conditions, such as chronic venous insufficiency (CVI), occlusive peripheral arterial disease or diabetes mellitus. Depending on how the condition presents, doctors distinguish between different types of venous leg ulcers or ulcers of the lower leg. The three most common types are:
Venous leg ulcers:
In order to diagnose a venous leg ulcer, it must be established that the ‘leg ulcer’ is caused by disrupted blood flow in the veins or, more specifically, chronic venous insufficiency. With regard to the localisation of the venous leg ulcer, a venous leg ulcer normally presents on the lower leg, generally at the level of the medial malleolus or the calf. It can develop on one or both sides of the leg. Some ulcer wounds can wrap all the way around the leg.
Arterial leg ulcers:
This is caused by a disruption to arterial circulation (peripheral vascular disease). Reduced supply of oxygen-rich blood means that even small wounds do not heal properly and get infected easily. Generally, an arterial leg ulcer presents on the toes or sole of the foot.
Mixed arterial-venous leg ulcers:
This is a term used by doctors to describe a leg ulcer caused by simultaneous constriction to both blood flows, i.e. both the venous and arterial vascular systems.
Venous leg ulcers are often associated with diabetes mellitus (diabetic foot). With this condition, there are multiple factors that make an ulcer more likely to occur: Arteriosclerosis, diabetic polyneuropathy and high sugar content in the interstitium.
However, there are other more rare causes such as a tumour which may be responsible for the impaired circulation and therefore cause a leg ulcer.
Venous leg ulcers – symptoms
The symptoms of a venous leg ulcer can vary depending on the severity of the condition and differ in some respects from the symptoms associated with an arterial leg ulcer.
The most common symptoms of venous ulcers include:
- Pain
- Swelling
- Itching
- Discolouration, e.g. redness
- Warmth in the affected area
- Unpleasant smell
- Hardened skin around the wound
- Haemosiderosis (iron deposits in the tissue)
- Spider veins
- Varicose veins
- White atrophy (small white areas, generally rough, scar tissue)
- Stasis dermatitis
- necrosis
- Lipodermatosclerosis (hardening of the subcutaneous fatty tissue)
- Moist or bleeding wound
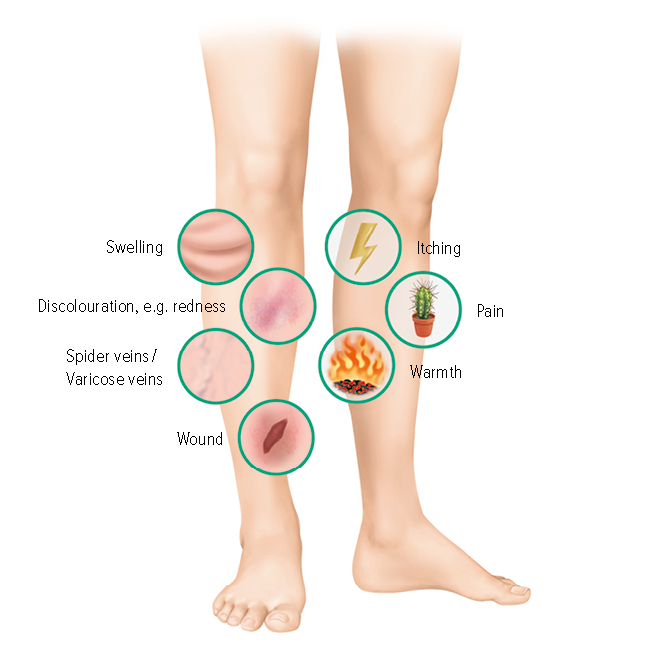
Complications associated with venous leg ulcers
The most common complication associated with a venous leg ulcer is an infection. If a wound is not cared for properly, bacteria can get in and cause an infection, which may make the wound worse and further delay healing. Deeper penetration of the bacteria leads to an infection of muscles or tendons, which may make more major surgery or even an amputation necessary. In serious cases, an infection can lead to erysipelas or sepsis. Both can be life-threatening. Furthermore, the risk of a heart attack or stroke is increased. Often, due to intensive wound treatment, allergies to ointments or disinfectant products can arise.
How common is a venous leg ulcer?
A venous leg ulcer is a condition that affects around 1% of the population. Women are more frequently affected than men. The risk of a venous leg ulcer increases with age and is higher for patients with chronic venous disorders.
How can I prevent venous leg ulcers?
You can do several things to help prevent venous leg ulcers. Action you can take ranges from increasing how much you move your body to healthy lifestyle changes and compression garments. Preventative measures:
- Preventative wearing of compression stockings
- Regular endurance sport (swimming, walking etc.)
- Vein exercises
- Lots of movement as part of everyday activities
- Moving between standing and sitting activities
- Investigating the first warning signs of vascular disease
- Optimal treatment of pre-existing diabetes
- A healthy diet
- No nicotine
- Avoiding being overweight
- Avoiding stress
- Wearing shoes that fit properly without any pressure points
- Regular foot care
The best way of preventing leg ulcers is to treat the underlying condition. This may, for example, mean that obese patients need to lose weight and become physically active or patients who have existing CVI need to wear compression stockings or take medication to manage diabetes. It is also important to look after the skin on your legs to prevent injuries. If you are injured, the injury needs to be treated quickly to promote healing.
Diagnosis of venous leg ulcers
A diagnosis of venous leg ulcers is normally made after a physical examination. The doctor examines the wound and looks for signs of infection. A medical history is also taken to establish any risk factors. An ultrasound is often carried out to check the blood flow in the leg and establish whether there is an underlying condition of the veins. Further diagnostic tests are possible, e.g. including:
- Ankle-Brachial Index (blood pressure in both arms and legs)
- Duplex ultrasound
- MRI or CT angiography
- Movement test
- Wound swab
- Blood tests (to check for diabetes, kidney issues etc.)
- Biopsy (if resistant to treatment)
Stages of venous leg ulcers
According to Knighton et al., there are six different levels of severity when it comes to chronic ulcers:
Level 1 Ulcer reaches the middle skin layer (epidermis and dermis)
Level 2 Subcutaneous ulcer
Level 3 Ulcer reaches the tendons, bones, ligaments or joints
Level 4 Ulcer reaches the tendons, bones, ligaments or joints with additional inflammation (abscess and/or infection of the bone marrow)
Level 5 Ulcer reaches the tendons, bones, ligaments or joints with additional dead tissue (necrosis) in the wound
Level 6 Ulcer reaches the tendons, bones, ligaments or joints with additional dead tissue (necrosis) in the wound and surrounding tissue
Leg ulcers: Treatment
What can I do to treat venous leg ulcers? The type of treatment for venous leg ulcers depends on the severity of the condition. In moderate cases, in addition to venous leg ulcer wound care, compression therapy is generally required. This forms the basis of the treatment and helps to increase blood flow to the veins and reduce pressure in the veins. This can help to promote wound healing. In serious cases, special treatment or surgical intervention is necessary. Since chronic open wounds are always painful, all patients affected by this condition should receive suitable pain therapy. Ultimately, different treatment methods are often combined.
Treatment of the underlying circulation issue
- Adjustable compression wraps or elasticated rolls for decongestion
- Compression stockings or compression stocking system (Juzo Ulcer Pro)
- Regular wearing of compression garments
- Regular exercise, walking
- Treatment of any varicose veins
- Manual lymphatic drainage for oedema
- A healthy diet
- No nicotine
- Healthy blood pressure
- Potentially endovascular or vascular surgical procedures
- Medication to thin the blood and dissolve blood clots
Wound care
- Wound cleaning
- Rinsing with salt solution
- Debridement
- Removing dead, damaged or inflamed tissue
- wound dressings
- Slightly moist environment created with moist compresses, polymer membrane dressings, alginates, foam dressings, hydrocolloids, films, hydrogels
- Therapy for the wound edge environment
Surgical treatment
There are three main approaches here:
- Eliminating insufficient epifascial and transfascial venous sections (e.g. removing varicose veins)
- Ulcer surgery (e.g. shave therapy which creates a ‘new wound’ which then heals better)
- Fascia surgery: Involvement of the crural fascia
The last two approaches usually involve a subsequent split-thickness skin graft.
But when does a venous leg ulcer require surgical treatment? The rule here is that if the wound has not reduced in size within three months despite treatment or has not fully healed within a year, special treatment or surgical intervention is required.
Special treatment
In addition to compression therapy, wound care, medication and surgery, there are other procedures which can be used to treat chronic open wounds. This includes vacuum therapy, moist wound treatment and the use of skin replacement products.
Examples:
- Vacuum sealing
- Skin replacement therapy
- Plasma therapy
- Stem cell transplant
- Fat cell transplant
Help with venous leg ulcers by using compression therapy
For venous leg ulcers, consistent compression therapy is essential and is the most important treatment method. The gentle pressure from the outside interacts with the internal pressure of the vascular walls. This reduces the risk of the vein expanding. It helps to increase blood flow to the veins and reduce pressure in the veins. This can help to promote wound healing. Compression therapy can be achieved by wearing compression stockings or special dressings. A compression stocking supports the vessels from the outside. Circulation in the leg veins is optimised, preventing congestion and localised accumulation of the blood. The external pressure helps the venous valves to close more effectively and supports the functionality of the venous muscle pumps.
After a surgical procedure, wearing compression stockings reduces the risk of swelling and blood clots and promotes healing. Depending on the cause of the venous leg ulcer, long-term compression therapy is advisable as the risk of the condition recurring is high.
In order to have the best possible effect, the stockings should fit precisely. Therefore, they are measured by medical supply retailers.

Juzo Ulcer Pro
The compression stocking system for the treatment of venous leg ulcers
Special products
ACWs are an ideal starting point for ulcer treatment. This is because this type of compression garment is particularly easy to wear and can also be used to secure a separate wound covering if required. In addition, ACWs, such as the Juzo Compression Wrap or Juzo ACS Light, are an ideal size in case of swelling at the start of the therapy process.
For further ulcer care, patients can use the Juzo Ulcer Pro compression stocking system. This consists of two liner stockings (<CCL 1) for regular changing and a flat knit over-stocking (CCL 2). In combination, this results in compression class 3 pressure values. The liner stocking protects sensitive skin when putting on the over-stocking and can be used to firmly secure wound dressings and pads if needed.
Conclusion
Venous leg ulcers are painful. However, it is possible to reduce your risk of venous leg ulcers by paying attention to vein health and to the skin in the leg area. The treatment depends on the severity of the condition, but compression therapy is often the most important treatment method for venous leg ulcers.
If you notice signs of a venous leg ulcer, contact a doctor straight away to get a diagnosis and the best possible treatment.




